Varicocele and Male Fertility
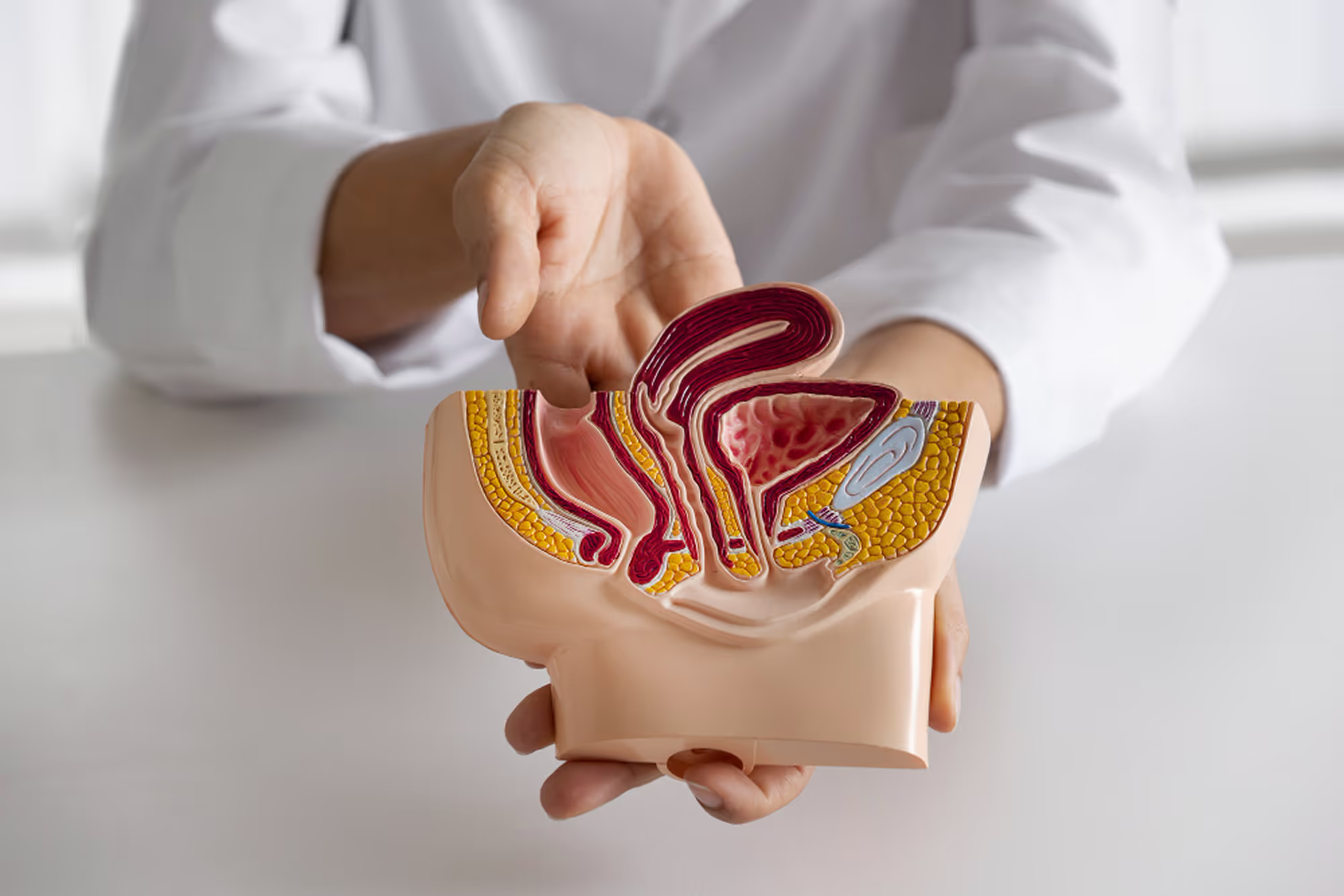
A varicocele is one of the most common and well-established causes of male infertility, yet it is also one of the most frequently underdiagnosed. A varicocele refers to abnormal dilation of the veins within the scrotum that drain blood away from the testes. These veins play a critical role in regulating testicular temperature and blood flow—two factors essential for normal sperm production.
At The Y Factor, varicoceles are evaluated as part of a diagnostic-first male fertility assessment, recognizing that their impact extends beyond sperm count alone and may influence motility, morphology, DNA integrity, and pregnancy outcomes.
What Is a Varicocele?
A varicocele develops when the valves within the scrotal veins fail to function properly, allowing blood to pool around the testes. This venous congestion disrupts the delicate testicular environment required for healthy sperm production.
Varicoceles most commonly occur on the left side due to differences in venous anatomy, though bilateral varicoceles are not uncommon. Severity ranges from small, subclinical varicoceles detectable only by ultrasound to larger varicoceles that can be felt on physical examination.
How Varicoceles Affect Male Fertility
Varicoceles impair fertility through multiple mechanisms that act together over time.

Testicular Temperature Regulation
The testes are positioned outside the body to maintain a temperature slightly cooler than core body temperature. Varicoceles interfere with this cooling mechanism, leading to elevated testicular temperature. Even modest temperature increases can disrupt sperm production and maturation.

How Common Are Varicoceles in Men With Infertility?
Varicoceles are found in a substantial proportion of men evaluated for infertility and are even more common among men with secondary infertility (difficulty conceiving after previously fathering a child). This prevalence highlights the importance of actively evaluating for varicoceles during male fertility assessment.

Signs and Symptoms of Varicocele-Related Fertility Issues
Many men with varicoceles have no symptoms. When present, symptoms may include:
- dull scrotal aching or heaviness
- discomfort that worsens with standing or activity
- visible or palpable scrotal veins
In many cases, infertility or abnormal semen analysis is the first indication that a varicocele is clinically relevant.
How Varicoceles Affect Sperm Quality
Evaluation typically begins with a semen analysis to assess sperm count, motility, and morphology, which helps determine whether a varicocele is affecting sperm production or function.

Why Varicoceles Are Often Missed in Fertility Evaluation
Varicoceles are frequently overlooked because:
- many men are asymptomatic
- physical exam findings can be subtle
- imaging is not routinely performed
- male evaluation is often delayed
Without targeted evaluation, varicoceles may remain undiagnosed despite their clinical significance.
How Varicocele-Related Fertility Issues Are Evaluated
Physical Examination
A focused examination by an experienced clinician may identify varicoceles, particularly under specific conditions.
Scrotal Ultrasound
Ultrasound confirms the diagnosis, assesses severity, evaluates testicular size, and identifies bilateral disease.
Semen Analysis and Hormonal Testing
Semen analysis reveals functional impact, while hormonal testing assesses testicular reserve and endocrine contribution.

Varicoceles and Pregnancy Outcomes
Varicoceles have been associated with:
- reduced natural conception rates
- prolonged time to pregnancy
- poorer assisted reproduction outcomes
- increased miscarriage risk in some cases
Understanding their role helps guide informed fertility planning.

Management Depends on the Individual Clinical Context
Not all varicoceles require intervention. Management depends on fertility goals, semen abnormalities, symptoms, and partner factors. Diagnostic clarity determines whether observation, optimization, or referral is appropriate.

When to Seek Evaluation for Varicocele and Fertility
Evaluation should be considered when:
- semen abnormalities are present
- infertility is unexplained
- scrotal discomfort exists
- future fertility is a concern
Schedule a Male Fertility Evaluation
The Y Factor provides comprehensive male fertility evaluation in Houston, focused on identifying varicocele-related contributors and guiding evidence-based care.