Semen Analysis for Male Fertility Evaluation
A semen analysis is the foundational diagnostic test for evaluating male fertility. It provides objective information about sperm production, quality, and function—factors that play a role in nearly half of all couples experiencing difficulty conceiving.Despite its importance, semen analysis is often misunderstood, underutilized, or misinterpreted. Many men receive a basic lab report without explanation, reassurance, or a plan—leading to unnecessary anxiety or missed opportunities for improvement.
At The Y Factor, semen analysis is treated as a clinical diagnostic tool, not a standalone lab test. Results are interpreted in context, connected to fertility goals, and used to guide thoughtful next steps rather than rushed conclusions.


What Is a Semen Analysis?
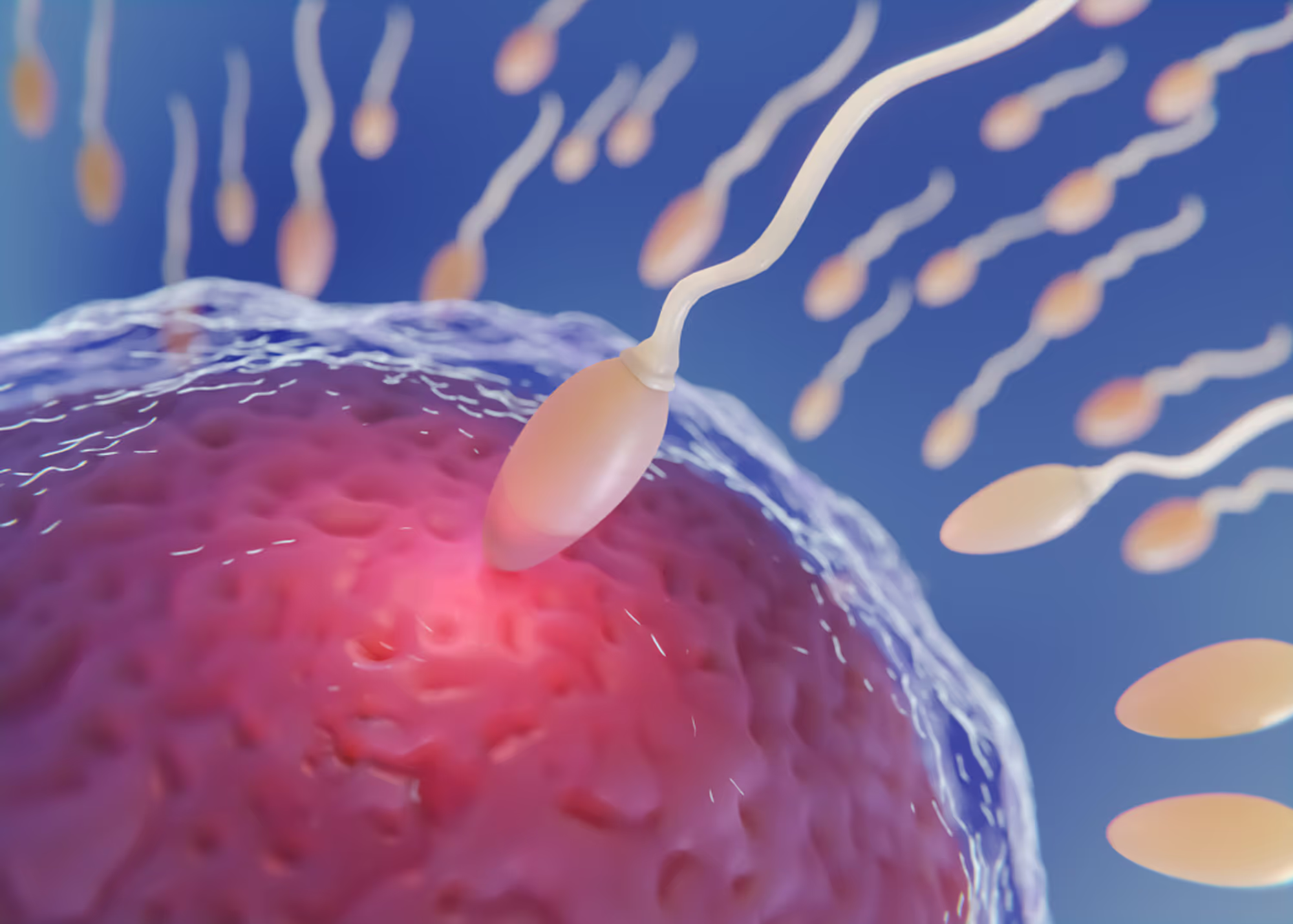
A semen analysis is a laboratory evaluation of a man’s ejaculate that assesses key characteristics of sperm and seminal fluid. It provides insight into how well sperm are produced, how they move, and how they are structured.
This test does not determine fertility on its own, but it offers essential data that informs whether additional evaluation, lifestyle optimization, medical management, or assisted reproductive planning may be appropriate.

Why Semen Analysis Matters in Fertility Evaluation
Male factor infertility contributes to infertility in approximately 40–50% of couples. Yet evaluation often focuses disproportionately on the female partner, delaying diagnosis and prolonging uncertainty.
A semen analysis:
- identifies treatable or reversible contributors
- helps avoid unnecessary procedures or delays
- provides baseline data for tracking improvement
- informs whether natural conception is likely or if additional support is needed
Importantly, semen quality can change over time. Testing offers a snapshot—not a permanent verdict.
What a Semen Analysis Measures
A comprehensive semen analysis evaluates several core parameters, each of which contributes to fertility potential.

Sperm Concentration (Count)
Sperm concentration measures how many sperm are present per milliliter of semen. Lower-than-expected counts may reflect:
- reduced sperm production
- hormonal influences
- testicular or ductal issues
- lifestyle or environmental factors
Concentration is interpreted alongside volume to calculate total sperm count.
Know More
Sperm Motility
Motility refers to the percentage of sperm that move and how effectively they progress forward. Because sperm must travel through the female reproductive tract, motility plays a key role in fertilization.
Reduced motility may be influenced by:
- oxidative stress
- infection or inflammation
- metabolic health
- varicocele or vascular factors
Motility abnormalities are often improvable once contributors are identified.
Know More

Sperm Morphology
Morphology assesses sperm shape and structure. While morphology receives a lot of attention, it must be interpreted carefully and in combination with other parameters.
Abnormal morphology does not automatically mean infertility, but it may guide decisions around timing, optimization, or assisted techniques if needed.
Know More

What a Semen Analysis Does Not Show
While valuable, semen analysis has limitations. It does not directly assess:
- sperm DNA integrity
- fertilization capability at the cellular level
- genetic or chromosomal abnormalities
- underlying causes of abnormal parameters
This is why interpretation and follow-up matter more than isolated numbers.

Who Should Consider Semen Analysis
Semen analysis is appropriate for:
- couples trying to conceive for 6–12 months without success
- men with a history of miscarriage with a partner
- men planning fertility preservation
- men with known risk factors (varicocele, testicular injury, hormone issues)
- men who want baseline fertility information before hormone therapy
Early testing often saves time and reduces unnecessary interventions.
How Semen Analysis Is Performed
Collection Options
Semen samples may be collected:
- on-site in a private clinical setting
- at home with proper timing and transport
The method depends on convenience, timing, and clinical context. Clear instructions are essential to ensure accurate results.
Handling and Timing Considerations
To optimize accuracy:
- abstinence period is typically 2–5 days
- samples should be analyzed promptly
- temperature and transport conditions matter
Improper handling can distort results, which is why clinical guidance is important.

Interpreting Semen Analysis Results
Numbers alone rarely tell the full story. Interpretation considers:
- all parameters together
- clinical history and age
- partner factors
- variability between samples
One abnormal test does not define fertility status. Trends and context matter.
.avif)
Why Abnormal Results Don’t Always Mean Infertility
Semen parameters fluctuate naturally due to:
- illness or fever
- stress
- sleep patterns
- recent lifestyle changes
Many abnormalities are temporary or reversible. Others may still be compatible with natural conception depending on severity and overall context.
.webp)
How Semen Analysis Guides Next Steps
Depending on results, next steps may include:
- lifestyle or metabolic optimization
- hormone evaluation
- scrotal ultrasound to assess anatomy or varicocele
- repeat testing to assess trends
- referral for assisted reproductive consultation when appropriate
The goal is to choose the least invasive, most effective path forward.
.avif)
When to Repeat or Expand Testing
Repeat testing may be recommended when:
- results are borderline or unexpected
- lifestyle changes are initiated
- treatment or optimization is underway
- fertility goals change
Additional testing may be considered when results suggest deeper contributors.
Schedule a Semen Analysis
The Y Factor offers comprehensive semen analysis in Houston with clinical interpretation and guidance—not just a lab result.
If you’re evaluating fertility, planning for the future, or seeking clarity about sperm health, scheduling a semen analysis is often the most informative first step.
Book an appointment to begin a fertility-focused diagnostic evaluation.
