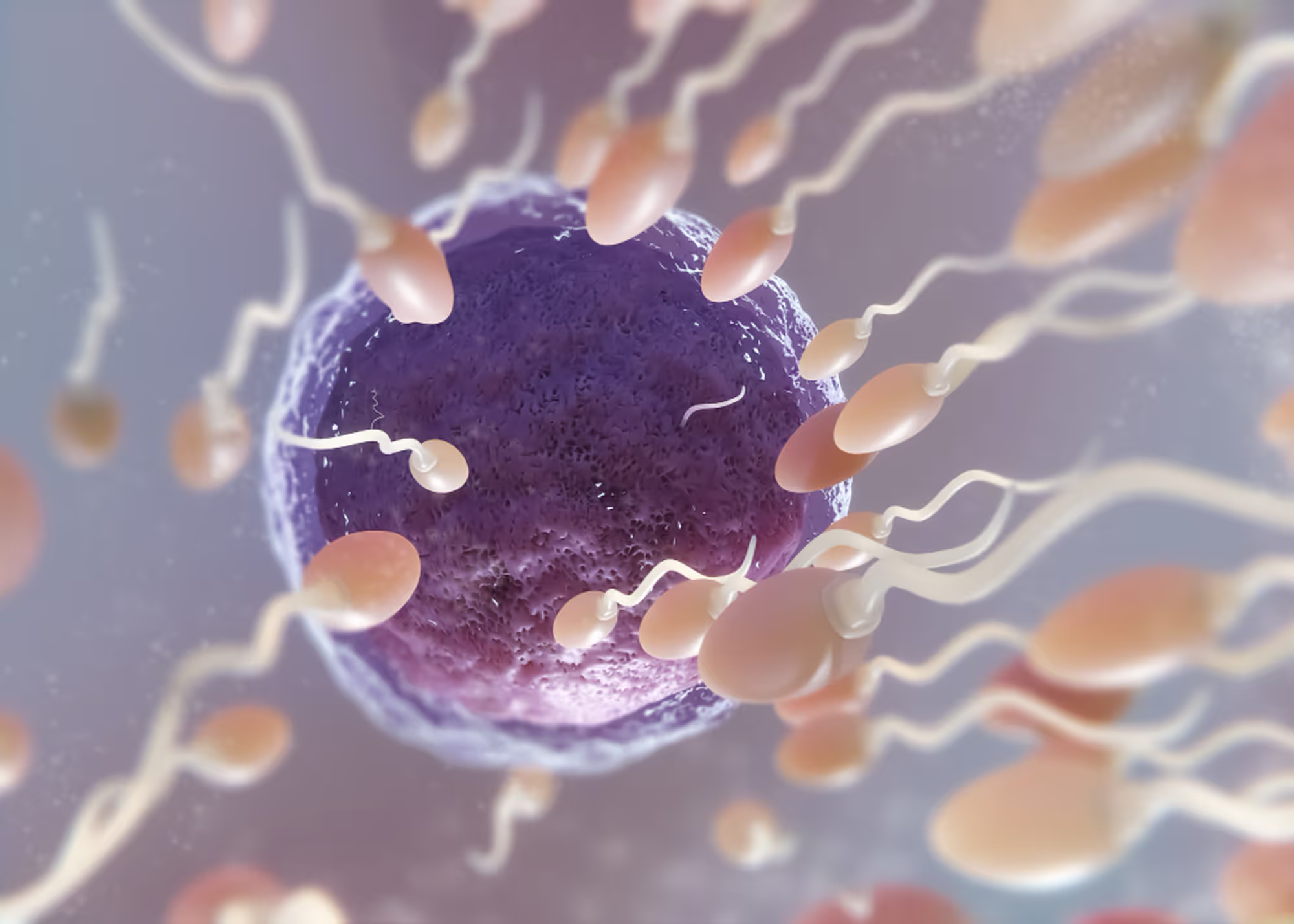
Low Sperm Count (Oligospermia): Causes, Evaluation, and Treatment Options
Low sperm count, medically referred to as oligospermia, is one of the most common findings during male fertility evaluation. It refers to a reduced number of sperm present in the ejaculate and can significantly affect the likelihood of achieving pregnancy. While low sperm count does not automatically mean infertility, it often warrants careful evaluation to determine the underlying cause and appropriate next steps.
At The Y Factor, low sperm count is approached through a diagnostic-first, evidence-based framework. Rather than focusing solely on the semen result itself, we aim to understand why sperm production or delivery is impaired and how that information should guide individualized care and family planning decisions.

What Is Low Sperm Count?
Low sperm count is typically defined as a sperm concentration below established reference ranges on semen analysis. Severity can vary widely and may include:
- mildly reduced sperm concentration
- moderately reduced sperm concentration
- severely reduced sperm concentration
- absence of sperm in the ejaculate
Importantly, sperm count is only one component of semen quality. Fertility potential depends on the combined interaction of sperm count, motility, morphology, and overall reproductive health.
How Sperm Count Affects Male Fertility
Sperm Count vs Overall Fertility Potential
Higher sperm counts generally increase the probability that sperm will reach and fertilize an egg. However, fertility is not determined by sperm count alone. Some men with mildly reduced sperm counts may still conceive naturally, while others with higher counts may face fertility challenges due to additional abnormalities.
Sperm count should always be interpreted in clinical context rather than in isolation.
Low Sperm Count vs Other Semen Abnormalities
Low sperm count may occur by itself or alongside other semen abnormalities, such as:
- poor sperm motility (reduced movement)
- abnormal sperm morphology (irregular shape)
When multiple abnormalities are present, fertility potential may be more significantly affected. Comprehensive evaluation helps clarify the degree of impact and guide management.
Common Causes of Low Sperm Count
Low sperm count can arise from a wide range of contributing factors. Identifying the underlying cause is critical to determining whether the condition is reversible, treatable, or requires advanced reproductive planning.
Testicular Causes of Low Sperm Count
Testicular dysfunction is one of the most common contributors to reduced sperm production. Potential causes include:
- prior testicular injury or trauma
- inflammation or infection
- varicoceles affecting testicular blood flow
- impaired testicular development or function
Damage to sperm-producing tissue can reduce sperm output even when hormone levels appear normal.
Common Causes of Low Sperm Count
Low sperm count can arise from a wide range of contributing factors. Identifying the underlying cause is critical to determining whether the condition is reversible, treatable, or requires advanced reproductive planning.
Testicular Causes of Low Sperm Count
We don’t prescribe testosterone until we understand why it’s low. Our providers conduct an in-depth clinical evaluation Testicular dysfunction is one of the most common contributors to reduced sperm production.
Potential causes include:
- prior testicular injury or trauma
- inflammation or infection
- varicoceles affecting testicular blood flow
- impaired testicular development or function
Damage to sperm-producing tissue can reduce sperm output even when hormone levels appear normal.
Hormonal Causes of Low Sperm Count
Hormones play a central role in regulating sperm production. Disruptions anywhere along the hormonal axis may impair spermatogenesis. Hormonal contributors may include:
- insufficient stimulation from pituitary hormones
- functional suppression related to obesity, stress, or illness
- hormonal imbalance despite normal testosterone levels
Because hormonal abnormalities may be subtle, testing is often required even in men without classic symptoms.
Anatomic and Structural Causes
Structural abnormalities can interfere with sperm production or transport. These may include:
- obstruction of the reproductive tract
- congenital absence or narrowing of sperm-carrying structures
- scarring from prior surgery or infection
In these cases, sperm may be produced but unable to reach the ejaculate in normal quantities.
Lifestyle, Metabolic, and Environmental Factors
Male fertility reflects overall health. Factors associated with reduced sperm count may include:
- obstruction of the reproductive tract
- congenital aobesity and metabolic dysfunction
- tobacco, alcohol, or substance use
- heat exposure to the testes
- environmental or occupational toxins
- chronic stress and inflammation
Addressing modifiable contributors may improve sperm parameters and long-term health.
How Low Sperm Count Is Diagnosed
The Role of Semen Analysis
Semen analysis is the cornerstone of diagnosing low sperm count. It provides objective measurement of:
- sperm concentration
- total sperm number
- motility and morphology
Results are compared against reference ranges and interpreted within the context of clinical history and fertility goals.
Why Repeat Semen Testing Is Often Necessary
Sperm production is dynamic and influenced by illness, stress, and lifestyle changes. Because of this variability, a single abnormal semen analysis does not always reflect a permanent condition.
Repeat testing is often recommended to:
- confirm persistent abnormalities
- assess trends over time
- guide further evaluation
Additional Evaluation After Low Sperm Count Is Identified
Hormonal Testing
Hormonal evaluation helps determine whether endocrine factors are contributing to low sperm production. Testing may assess:
- testosterone
- luteinizing hormone (LH)
- follicle-stimulating hormone (FSH)
Hormonal patterns provide insight into whether testicular dysfunction or regulatory issues are present.
Scrotal Ultrasound and Imaging
Scrotal ultrasound may be used to evaluate:
- testicular size and structure
- varicoceles
- masses or structural abnormalities
Imaging is selected based on semen results and physical findings.
Additional Testing in Select Cases
In certain situations, further testing may be considered to evaluate infection, inflammation, or genetic contributors. Testing is individualized and based on clinical relevance.

Low Sperm Count and Pregnancy Outcomes
Low sperm count may affect:
- time to conception
- likelihood of natural conception
- need for assisted reproductive techniques
Emerging evidence also suggests that severe sperm abnormalities may be associated with pregnancy loss or adverse outcomes, highlighting the importance of thorough male evaluation.

Management Depends on the Underlying Cause
There is no single treatment for low sperm count. Management depends on identifying the cause and may include:
- lifestyle and metabolic optimization
- medical therapy
- procedural intervention when appropriate
- coordination with reproductive specialists
The goal is to provide realistic expectations and evidence-based guidance.
.avif)
When to Seek Evaluation for Low Sperm Count
Men should consider evaluation if:
- semen analysis shows low sperm count
- pregnancy has not occurred after appropriate attempts
- there is a history of testicular injury, surgery, or illness
- future fertility is a concern
Early evaluation often leads to more informed and efficient care.
Schedule a Male Fertility Evaluation
The Y Factor provides comprehensive male fertility evaluation in Houston, with a focus on diagnostic accuracy, clinical oversight, and individualized care planning.
Appointments can be scheduled online or by contacting our clinic directly.