Poor Sperm Motility (Asthenozoospermia): Causes, Evaluation, and Treatment Options
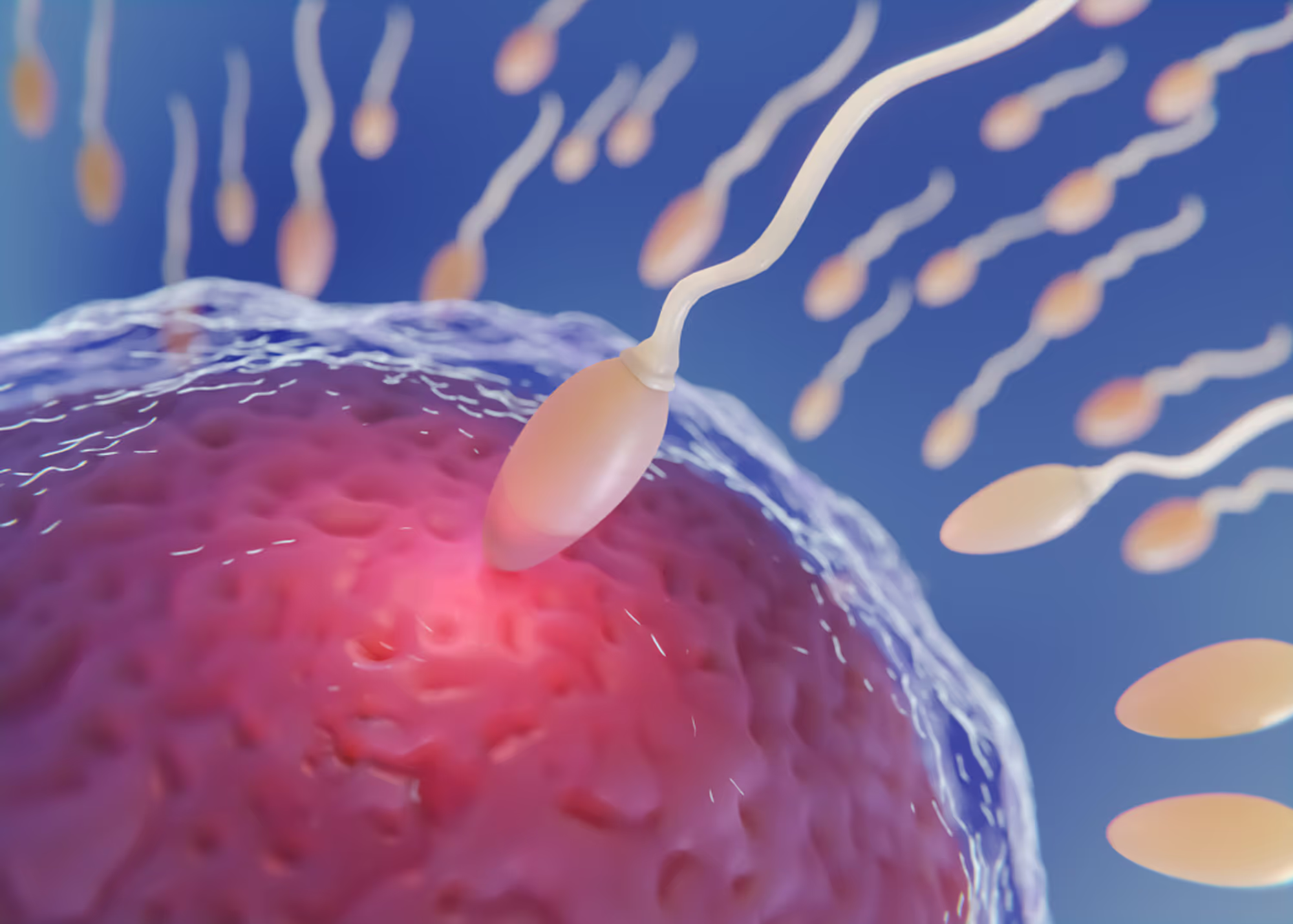
Poor sperm motility, medically referred to as asthenozoospermia, is a common and often underrecognized contributor to male infertility. Sperm motility refers to the ability of sperm to move effectively through the female reproductive tract in order to reach and fertilize an egg. Even when sperm count is normal, impaired motility can significantly reduce the likelihood of conception.
At The Y Factor, poor sperm motility is evaluated through a diagnostic-first, evidence-based approach. Rather than treating semen abnormalities in isolation, we focus on identifying the underlying biologic, hormonal, and environmental factors that impair sperm movement and using that information to guide individualized care and family planning decisions.

What Is Poor Sperm Motility?
Sperm motility describes how well sperm move. For fertilization to occur naturally, sperm must travel through the cervix, uterus, and fallopian tubes to reach the egg. This requires coordinated, forward (progressive) movement.
Poor sperm motility occurs when a high proportion of sperm:
- move slowly
- move erratically
- fail to move forward
- are completely immotile
A diagnosis of poor sperm motility is made based on semen analysis results compared against established reference ranges.
Why Sperm Motility Is Critical for Fertility
How Sperm Motility Affects Natural Conception
Even with adequate sperm count, sperm that cannot move effectively may never reach the egg. Progressive motility—the ability of sperm to move forward in a straight or slightly curved path—is particularly important for natural conception.
Reduced motility may:
- prolong time to conception
- reduce likelihood of fertilization
- increase reliance on assisted reproductive techniques
Sperm Motility vs Sperm Count and Morphology
Sperm motility is just one component of semen quality. Fertility potential depends on the interaction of:
- sperm count (quantity)
- sperm motility (movement)
- sperm morphology (shape)
Some men have isolated motility issues, while others have combined abnormalities. Comprehensive evaluation helps determine the degree of impact and appropriate next steps.
Types of Sperm Motility Abnormalities
Reduced Progressive Motility
Progressive motility refers to sperm that move forward efficiently. Reduced progressive motility means that fewer sperm are capable of reaching the egg, even if they are alive and moving.
Non-Progressive or Immotile Sperm
Some sperm may move but fail to progress forward, while others may not move at all. High proportions of non-progressive or immotile sperm are associated with lower fertility potential.
Common Causes of Poor Sperm Motility
Poor sperm motility can arise from a wide range of contributing factors. Identifying the cause is essential to determining whether the condition is reversible, treatable, or requires advanced reproductive planning.
Testicular and Epididymal Causes
Sperm motility depends on proper sperm development and maturation. Contributors may include:
- impaired sperm development within the testes
- abnormal maturation in the epididymis
- testicular injury or inflammation
Structural abnormalities or impaired blood flow may also affect sperm quality.
Hormonal and Metabolic Causes
Hormones regulate sperm production and maturation. Hormonal contributors to poor motility may include:
- testosterone imbalance
- pituitary dysfunction
- metabolic conditions such as obesity or insulin resistance
Hormonal abnormalities may exist even in men without classic symptoms.
Oxidative Stress and Inflammation
Oxidative stress occurs when reactive oxygen species damage sperm cell membranes and internal structures. Inflammation within the reproductive tract may impair sperm function and motility.
Sources of oxidative stress may include:
- infection or inflammation
- metabolic dysfunction
- environmental toxin exposure
Lifestyle and Environmental Factors
Sperm motility is sensitive to overall health and environmental exposure. Contributors may include:
- tobacco, alcohol, or substance use
- heat exposure to the testes
- chronic stress
- poor sleep
- nutritional deficiencies
Addressing modifiable factors can sometimes improve motility over time.
How Poor Sperm Motility Is Diagnosed
The Role of Semen Analysis
Semen analysis is the primary tool for assessing sperm motility. It evaluates:
- percentage of motile sperm
- percentage of progressively motile sperm
- overall semen quality
Results must be interpreted within clinical context and compared against established reference ranges.
Why Repeat Testing Is Often Necessary
Sperm production and motility fluctuate over time and may be temporarily affected by illness, stress, or lifestyle changes. Repeat semen testing is often recommended to:
- pconfirm persistent abnormalities
- assess trends
- guide further evaluation
Additional Evaluation After Poor Motility Is Identified
Hormonal Testing
Hormonal evaluation may assess testosterone and related hormones to identify endocrine contributors to impaired motility.
Scrotal Ultrasound
Scrotal ultrasound may be used to evaluate:
- testicular structure
- varicoceles
- abnormalities affecting blood flow or temperature regulation
Semen Culture and Inflammatory Assessment
When infection or inflammation is suspected, semen culture or additional testing may be recommended to identify treatable contributors.
Poor Sperm Motility and Pregnancy Outcomes
Poor sperm motility may:
- reduce likelihood of natural conception
- increase time to pregnancy
- necessitate assisted reproductive techniques
Emerging evidence also suggests that severe motility defects may be associated with adverse pregnancy outcomes, reinforcing the importance of thorough evaluation.

Management Depends on the Underlying Cause
There is no single treatment for poor sperm motility. Management depends on identifying contributing factors and may include:
- lifestyle and metabolic optimization
- addressing inflammation or infection
- hormonal management when indicated
- procedural intervention in select cases
Treatment plans are individualized based on diagnosis and reproductive goals.

When to Seek Evaluation for Poor Sperm Motility
Men should consider evaluation if:
- semen analysis shows reduced motility
- pregnancy has not occurred despite appropriate attempts
- there is a history of testicular injury or infection
- future fertility is a concern
Early evaluation often leads to more efficient and informed care.
Schedule a Male Fertility Evaluation
The Y Factor provides comprehensive male fertility evaluation in Houston, focused on diagnostic accuracy, clinical oversight, and individualized care planning.
Appointments can be scheduled online or by contacting our clinic directly.