Low Testosterone and Male Fertility
Low testosterone and male fertility are closely connected, yet the relationship is often misunderstood. Testosterone plays a critical role in male reproductive health, but the way it influences sperm production is more complex than many men realize. As a result, men experiencing symptoms of low testosterone may unknowingly face fertility challenges, while others may receive treatment that unintentionally compromises their reproductive potential.
At The Y Factor, low testosterone is evaluated within the broader context of fertility and family planning. Understanding how testosterone functions within the male reproductive system allows men to make informed decisions that align with both their health goals and future family plans.


The Relationship Between Testosterone and Fertility
Testosterone is essential for male sexual development, libido, and physical health. However, the testosterone measured in blood tests represents only one part of the hormonal environment that supports sperm production.
Within the testes, testosterone levels are significantly higher than in the bloodstream. This local testosterone environment is necessary for normal sperm development. Disruption at any level—whether from low production, impaired signaling, or external hormone exposure—can negatively affect fertility.
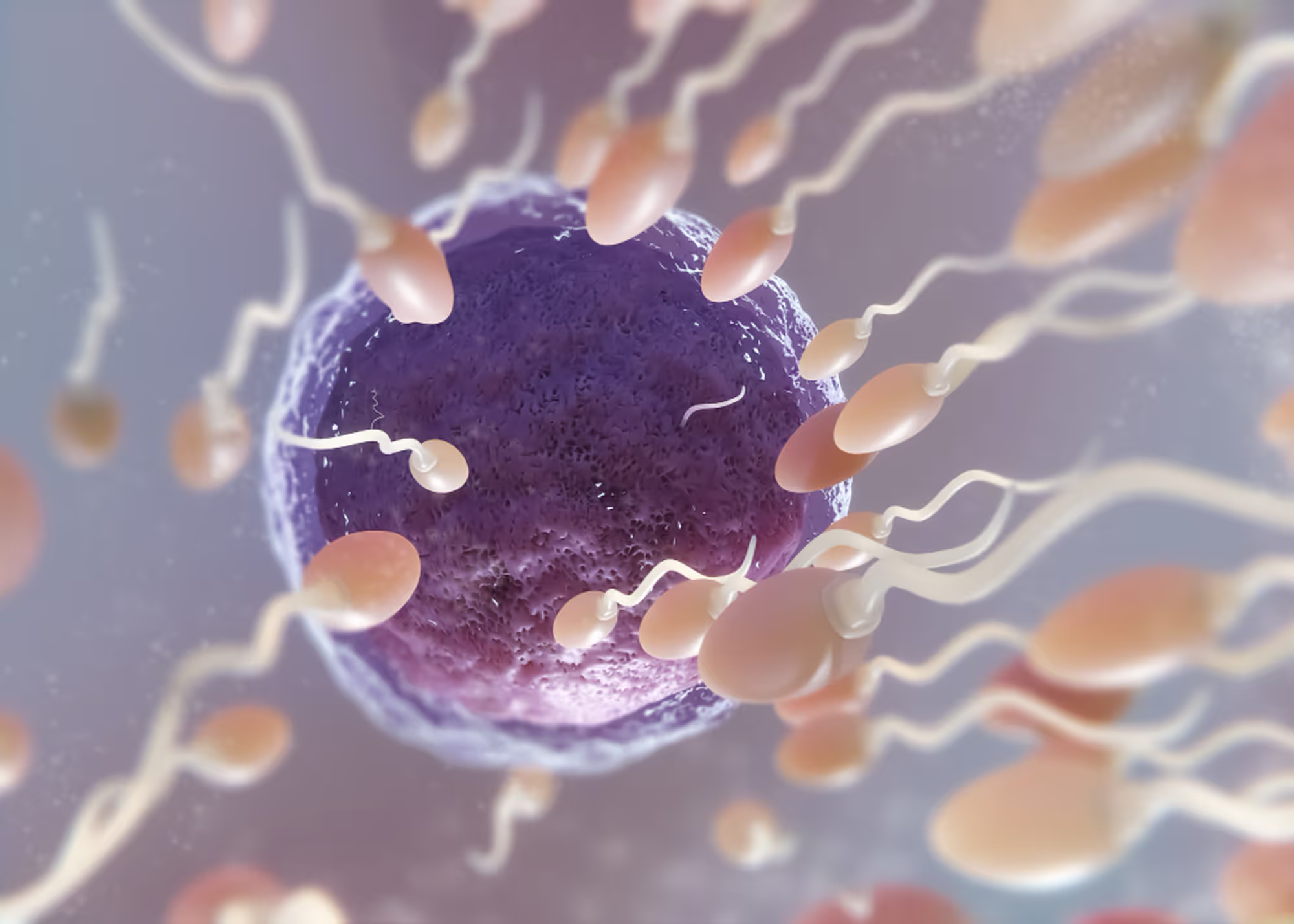
How Testosterone Supports Sperm Production
Sperm production occurs in the seminiferous tubules of the testes and requires:
- adequate local testosterone levels
- proper signaling from the brain
- a supportive metabolic and hormonal environment
Testosterone works in concert with other hormones to regulate the maturation of sperm cells. Even subtle hormonal disruptions can impair sperm count, motility, or morphology.

Why Low Testosterone Can Affect Fertility
Low testosterone may affect fertility in several ways:
- reduced stimulation of sperm production
- impaired maturation of sperm cells
- decreased libido and sexual frequency
- altered testicular environment
However, the degree of fertility impact depends heavily on the cause of low testosterone, not just the testosterone level itself.
Different Causes of Low Testosterone Have Different Fertility Implications
Understanding the underlying cause of low testosterone is essential when fertility is a concern.
Primary Hypogonadism and Fertility
In primary hypogonadism, the testes are unable to produce adequate testosterone despite proper signaling from the brain. Because sperm production also occurs in the testes, fertility impairment is often significant.
Men with primary hypogonadism may experience:
- reduced sperm production
- abnormal semen parameters
- infertility
Early evaluation helps determine whether fertility preservation or assisted reproductive options may be needed.
Secondary Hypogonadism and Fertility
In secondary hypogonadism, the brain fails to signal the testes adequately. In these cases, the testes may still have the capacity to produce sperm if proper stimulation is restored. Fertility potential may be preserved, making accurate diagnosis especially important.
Functional Low Testosterone and Fertility
Functional low testosterone is caused by metabolic, inflammatory, or lifestyle-related suppression. Because the reproductive system remains structurally intact, fertility impairment may be reversible once underlying stressors are addressed.
This category represents a critical opportunity for early intervention.

Symptoms That Suggest Hormonal and Fertility Overlap
Men may experience overlapping symptoms that suggest both hormonal imbalance and fertility issues, including:
- reduced libido
- erectile dysfunction
- fatigue
- difficulty conceiving
- abnormal semen analysis results
These symptoms warrant comprehensive evaluation rather than isolated treatment.
.avif)
Why Testosterone Levels Alone Do Not Tell the Full Fertility Story
Normal blood testosterone levels do not guarantee normal sperm production, and low testosterone does not always mean infertility. Fertility depends on:
- local testicular testosterone levels
- hormone signaling patterns
- sperm quality and genetic integrity
Relying solely on blood testosterone levels can be misleading.
How Testosterone Is Evaluated in Men Concerned About Fertility
Hormone Testing
Hormonal evaluation includes testosterone and related hormones that regulate sperm production. Testing is timed and repeated to ensure accuracy.
Semen Analysis and Reproductive Assessment
Semen analysis provides direct insight into fertility potential by measuring:
- sperm count
- motility
- morphology
Combining hormonal and semen data allows for a more complete assessment.
.avif)
The Impact of Testosterone Therapy on Fertility
External testosterone therapy can suppress the body’s natural hormone signaling, leading to reduced sperm production or even complete absence of sperm in the ejaculate.
This is why men who may want children in the future should never start testosterone therapy without a fertility-aware evaluation.
Why a Diagnostic-First Approach Matters
A diagnostic-first approach ensures that:
- underlying causes are identified
- fertility risks are understood
- treatment decisions align with long-term goals
This approach avoids unnecessary tradeoffs between symptom relief and reproductive potential.


When Men Should Seek Evaluation
Men should consider evaluation if they experience:
- symptoms of low testosterone
- difficulty conceiving
- abnormal semen analysis
- plans for future family building
Early evaluation expands options and reduces the risk of unintended fertility loss.
Schedule a Fertility-Focused Hormonal Evaluation
The Y Factor provides comprehensive hormonal and fertility evaluation in Houston, integrating diagnostic testing, clinical oversight, and individualized care planning.